A visit from The Joint Commission can be daunting, due to the importance of passing the inspection and obtaining accreditation for your medical facility.
However, earning accreditation from The Joint Commission provides many benefits; most significantly, it proves that your medical facility puts patients first, because the majority of The Joint Commission’s standards focus on patient safety and quality of care. Other advantages of accreditation include risk management, increased community confidence, reduction of liability insurance costs, and Medicare certification.
The Joint Commission estimates that 15 to 20 million reusable endoscopes are used in healthcare organizations; due to the invasive nature of these endoscopes, they can easily retain contaminated material if not correctly reprocessed. To help prevent the spread of infectious disease, The Joint Commission has set standards for managing endoscope reprocessing environments. They focus on three key areas: physical space, ventilation, and documentation/training.
To clean effectively, follow these directions in conjunction with your facility’s infection control protocol:
Ensure the area is the appropriate size for the volume of equipment.
All staff should always don suitable personal protective equipment (PPE) before entering the area.
Critical areas, cleaning supplies, and storage areas should be clearly labeled.
There must be an eyewash station and hand wash station, both easily accessible.
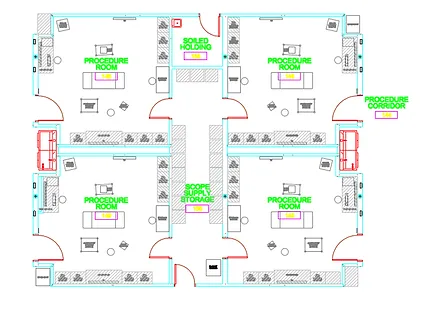
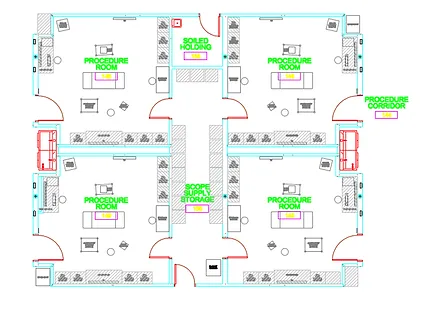
“Clean” areas should be separate and distinct from “dirty” areas, with suitable storage areas for clean endoscopes and other equipment.
The endoscope storage cabinets should have doors, be clean, free of debris, dry, and off of the ground.
The route from the processor to the cabinet should not cross through the soiled processing area.
The exhaust should be vented directly outside.
There should be negative air pressure to the surrounding areas.
A minimum of 10 air exchanges per hour are recommended, with at least two of those exchanges being with fresh, outside air.
Staff should know how many endoscopes are in the department.
Knowledge of maintenance procedures and frequency of maintenance should be exhibited by all staff.
All staff should be able to point out where the guidelines and evidence-based practices are located.
Periodic training should be provided to all staff, who should be able to show that they were appropriately trained using proper guidelines
Following these guidelines will strengthen patient care and provides the added benefit of helping your medical facility obtain accreditation from The Joint Commission.

We recommend using quaternary ammonium compounds for disinfecting the components of your scope cabinet.
While not suitable for cleaning the surface of your cabinet, bleach can be used on certain components if so desired.
Drip trays can be processed in or out of the cabinet, although we do recommend removing the tray in order to reach every surface.
Clean and disinfect the drip tray in the same manner as outlined above, taking care to dry completely before replacing.
The scope holders (including Secure-A-Scope™) should regularly be cleaned with a mild, non-abrasive detergent and then disinfected with a quaternary ammonium compound or bleach.
MASS™ truHEPA™ filters should be replaced every six months. MASS™ Medical Storage’s service team is available for this routine maintenance.
Parts to remember:
Door handle
Nylon door pull (tall cabinets only)
EUS holder, including the adjustment knob
Fan activation switch (if present)
“Benefits of Joint Commission Accreditation.” The Joint Commission. August 28, 2015. Available at: https://www.jointcommission.org/benefits_of_joint_commission_accreditation/. Accessed August 9, 2016.
Schumacher, P. “Tips for improving endoscope reprocessing and preventing the risk of infection.” Joint Commission Online. April 9, 2014. Web. Available at: http://www.jointcommission.org/assets/1/23/jconline_april_9_14.pdf. Accessed August 9, 2016.
